The 4 Stages of Healing
Author: Stephanie Biddell, Registered Physiotherapist
Updated: May 13, 2024
Have you ever wondered why after an injury some injuries take longer to heal than others? Or what happens at the cellular level during tissue recovery? The aim is to help you understand the processes of injury as much as possible and the reasoning for swelling or the length of healing. This article will take you through the body’s natural stages of healing, discuss the risk factors that prolong healing, and provide insight into rehab tips for appropriate rehab. As our scientific understanding advances, we gain deeper insights into the complexities of the body's healing process. This article has been updated to reflect some of the most recent findings in this field as of 2024.
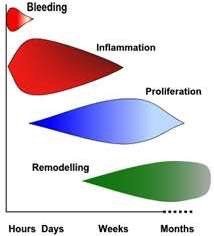
Generally speaking, the body’s different tissues (muscle, tendons, ligaments, cartilage, etc) follow the 4 stages of healing which comprise of Bleeding, Inflammation, Proliferation and Remodelling. Through these stages, the injured tissue will be destroyed and replaced by living tissue in the body. It is important to note that the healing phases are not mutually exclusive to their time frames and tend to overlap as you can see in Figure 1.
Figure 1. Adapted from Watson, (2006). The four stages of tissue repair. The stages overlap to highlight that there is a transition between the stages.
Stage 1. Bleeding
This is a short stage that occurs directly after an injury which focuses on protection and reaction so that the initial injury can be managed. This stage can last up to 24 hours and depends on the extent of the soft tissue injury, which structures have been injured, and the management.
There are many different cells that come rushing in to prevent and stop the bleeding. Thrombocytes are cells that help from clots and trigger vasoconstriction. Whereas platelets assist in clot formation. Lastly, leukocytes- which are a type of white blood cell which protect against foreign bodies and help fight any infection present. In this stage a clot is formed while leukocytes begin to remove foreign particles.
Recent research emphasizes the importance of effective management of this stage to set a solid foundation for the subsequent stages of healing. An adequate response to this initial trauma can help minimize complications and improve overall healing outcomes.
Stage 2. Inflammation
This stage focuses on protection and early repair and overlaps with Stage 3. Typically, inflammation presents with swelling, bruising, increased temperature, pain and loss in function at the injury site. While inflammation has traditionally been viewed as a process to be minimized, new research is uncovering its essential role in paving the way for tissue regeneration. Scientists are now exploring ways to harness the body's inflammatory response to enhance healing.
Protection
When cells are injured they release chemicals that stimulate the inflammatory process. The aim of this stage is to stimulate and regulate inflammation through vasodilation by sending lots of blood, oxygen and nutrients to the site. Due to this vasodilation it causes redness and swelling secondary to the blood rushing to the site!
This stage activates pain pathways where pain sends messages from the injury site to the brain- which then allows the brain to send signals to release chemicals or signal the injury to prevent further movement to enhance protection. Phagocytosis occurs which is a protective mechanism where white blood cells engulf foreign bodies to prevent infection.
Early Repair
This initiates the transition from inflammation to the proliferation phase. The inflammatory cells stay around so that when the proliferation starts, there is an overlap.
Stage 3. Proliferation
Proliferation means to “reproduce rapidly”. This is the first of the two major rebuilding stages. The phagocytes will start to leave and therefore inflammation will reduce.
Proliferation can start between 24-48 hours after an injury, and last up to 3 weeks once the bulk of the scar tissue is formed. This stage is where cells which are commonly referred to as “blasts” cells will come to the area to change the fibrin like matrix into a more structured matrix. “Blasts” means to build new tissue. Here, the fibrin matrix from the bleeding and inflammation state would be replaced by “immature” disorganized tissue.
In addition, new blood cells will start to form at the injured site- I.e. if one broke a bone, the blood vessels may have been broken at this time and therefore new vessels will form in the healing process. The blasts cells will lay down new tissue (whether it’s bone, muscle, cartilage, etc) which are “immature”- meaning that they cannot withstand the final forces yet.
Researchers are studying the factors that can influence the proliferation stage, such as diet, exercise, and even psychological stress. These insights could open up new ways to support and expedite this critical stage of healing.
Stage 4. Remodeling Stage
This stage is crucial to allow the “immature” tissue that was laid down to be converted to a more mature, organized and structured matrix. This process can last between months and even years depending on the tissue type! The cells take the disorganized immature tissue from the proliferation stage and will align the tissue in an organized, linear manner to construct the final tissue type. The final tissue type is what’s able to withstand the forces that go through that particular tissue during kinetic movement.
With the analogy of spaghetti, think of cooked spaghetti versus organized uncooked spaghetti that is found in the box. When it comes to immature tissues during the proliferation stage, the tissues are unorganized like a bowl of uncooked spaghetti. Whereas in the remodelling stage, the tissues finalize their linear matrix structure like in a box of uncooked spaghetti- and that is the ultimate goal to provide functional movement.
Current studies are investigating how various interventions, including physical therapy and nutritional supplementation, might enhance the remodeling process, improving both the speed and quality of tissue repair.
Now that you have learnt about the different and overlapping stages of general healing, let’s discuss the risk factors that may contribute to this process.
Image: AI depiction of the 4 stages of bone healing, from initial break to remodelled.
Risk Factors for Healing
The majority of the following risk factors are related to metabolic activity and the stages of healing:
Age
As we age our tissues develop and adapt at a slower pace. In addition, one’s metabolism slows down which has a cascade effect on healing.
Genetic Factors
Particularly with tendon injuries, genetics increase susceptibility. In addition, genetic clotting issues will effect and may prolong the bleeding stage.
Substance use
Previous use of steroids or overuse of drugs/ alcohol has a negative effect on healing as the fatty deposits impair the nutrients being delivered to the area.
Previous injury
Previous attempts of healing leaves the tendon not as intact as it once was.
Metabolic Influence
Smoking, diabetes, kidney function or eating disorders may have less efficient metabolic processes and effective blood supply to the area
Obesity
One may be more prone to infection or increased tendon fibre diameter which in turn leads to increased stiffness.
Activity levels
Too little or too much to allow the new tissue to bond if it is overstretched or not stressed enough.
How can rehab help?
Rehabilitation can provide education and guidance along the way to assist and promote effective healing by guiding individuals along their recovery. It is essential that in every stage of healing the treatment and rehab is specific and safe. As the injury progresses through the stages of healing, the treatment & rehabilitation has to progress accordingly. Physiotherapists can assist with the following:
Pain management and getting pain under control. This is a vital first step as pain can be quite the limiting factor to progression!
Education: Depending on the tissue that has been injured, a physiotherapist will be able to provide you with desired load management. It is common practice to immobilize the joint to prevent further damage and the patient to experience pain. The other benefits to immobilizing include decreased healing time, increased growth of blood vessels and stronger connective tissue. It is important to get the timing right for immobilization of the joint. If you remove the immobilization too early the redevelopment of new tissue and blood vessels can be immature and fragile. On the contrary, if you leave the immobilization for a prolonged period of time, the muscles will waste away and cause functional issues during late stage rehab. With education, a physiotherapist is able to educate you on the different tissues that have been affected and assist with appropriate timing of progression.
Exercise is vital, but has to be within tissue limits. A good indicator of this is pain and if monitored well, then the healing process can be accelerated within the range of movement at the site of injury. Exercise stimulates blood flow, allows for lineation of fibres, and ensures the muscle is strong to endure future loads. If there is too much blood in the area and swelling then this hematoma can create an element of fibrosis (less elastic) and can increase stiffness which leads to a delay in healing. Crucially, a lack of exercise in this healing process will further delay as the hematoma does not disperse efficiently and the newly laid muscle tissue does not contract and relax as efficiently as desired muscle tissue.
Mobility aids: It is encouraged to mobilize frequency within the surgeon’s protocol. Using an aid like crutches or a walking frame for the first time can be daunting, limiting or cause stiffness in different areas, however it is very important to frequently move in a safe manner.
Hydrotherapy: can encourage early loading through the legs without causing too much stress through the bones.
Rehabilitation techniques are continually evolving as we learn more about the body's healing process. Recent developments have highlighted the importance of personalized rehabilitation programs that take into account an individual's specific injury, overall health, and lifestyle.
Recap
Injuries are common and there is a natural process that the body encounters after an injury. This process can identify problems that impede healing, such as repeated trauma, inhibited response (potentially from risk factors) or delayed reactions. The aim of physiotherapy, in this case, would be to assist in stimulating the healing process through education and guidance. It is important to note that doing too much too soon will inhibit the process, likewise by not doing enough! Thus, it is important to have the right therapy at each stage! Chipperfield Physiotherapy can get your healing journey on track ASAP! Click to book an appointment below!